Trigger Finger Treatment and Management
Otherwise known as stenosing tenosynovitis, trigger finger is a condition where one of the fingers gets stuck in a bent position.
Depending on the severity, noninvasive treatments, injections, trigger finger surgery, or medications might be recommended.
Trigger finger can result from forceful use or the repeated movement of the thumb or finger. Other medical conditions like gout, rheumatoid arthritis, and diabetes can also cause trigger finger. Firmly grasping something (like a power tool) for a long period might also result to trigger finger.
Musicians, farmers, and industrial workers are susceptible to trigger finger as they are likely to do repeated thumb and finger movements. Repeated lighter use can also put smokers at risk of developing trigger finger. The condition is more common in individuals who are 40 to 60 years of age.
Telltale signs that point to trigger finger can include the following:
Physical examination of the fingers and hands is done in order to diagnose trigger finger. In some instances, the finger can become swollen and a bump over the joint of the palm will sometimes manifest.
The finger can also become locked in a bent position and may become painful and stiff. Lab tests and X-rays are not necessary to diagnose the condition.
Stretching exercises
Gentle exercises might be recommended to help maintain finger mobility.
Heat or ice
Some patients observe improvements when icing the palm several times daily. Others on the other hand benefit more from warm water soaks done first thing in the morning.
Splint
The doctor might have the patient wear a splint at night to keep the finger affected in an extended position. Apart from helping ensure the patient’s finger does not curl while asleep, splints can help to rest the tendon.
If the patient has severe symptoms and does not respond well to conservative treatments, the following will likely to be suggested.
Surgery
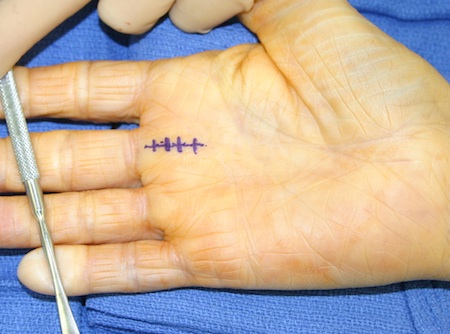
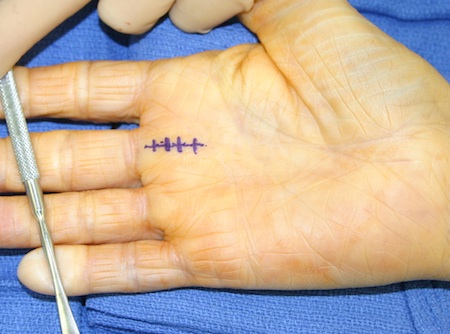
Usually done in the operating room, trigger finger surgery involves working through a small incision done near the base of the finger affected. The surgeon will then cut open the section of the tendon sheath that is constricted.
Percutaneous release
This procedure will entail numbing the patient’s palm before a sturdy needle is inserted into the tissue around the affected tendon. When the needle and the finger are moved, the constriction blocking the tendon’s smooth motion will be eradicated.
Steroid injection
To allow the tendon to move freely and to reduce inflammation, a steroid medication will be injected into the tendon sheath. This is oftentimes the most common treatment alternative chosen because it has been proven effective in as much as 90 percent of the patients. This option however is not advisable for patients with diabetes.
Recovery time will actually depend on the severity of the condition. In some cases, treatment choice can also affect recovery period (for instance, splinting may take at least 6 weeks). However, in most cases, patients will recover within a few weeks with rest and anti-inflammatory medications.
